COVID-19 and long COVID may be linked to impaired sensory neurons, a recent study Massachusetts Institute of Technology (MIT) study finds.
COVID-19 and long COVID may be linked to impaired sensory neurons, a recent study Massachusetts Institute of Technology (MIT) study finds.
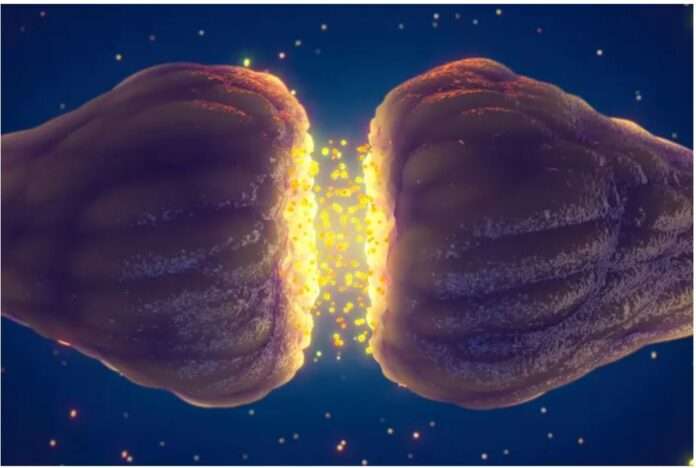
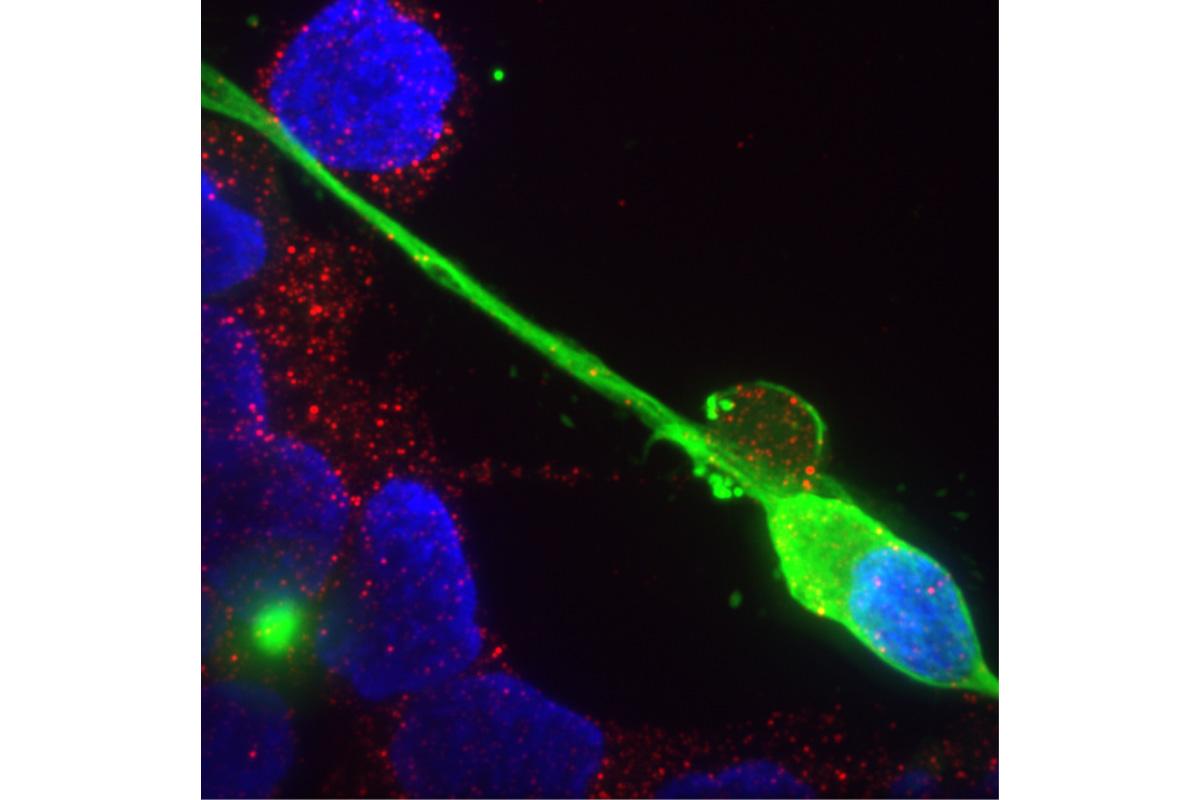
Sensory neurons are responsible for smell, taste, touch, pain, and changes in temperature. Damage to them may lead to impaired senses.
Surprisingly, the study found that infected neurons released viral proteins like the spike protein and nucleocapsid proteins rather than the virus releasing them.
Not all neurons were infected. All lab-made neurons were exposed to the Wuhan, delta, and omicron strains, but only up to 30 percent of the neurons were infected, with the omicron variant having the lowest infection rate.
Sensory Symptoms in Long COVID and Vaccine Injuries
Some doctors have suspected that the sensory problems, such as lost or impaired smell, taste, and hearing, and muscle pains, numbness, burning, and electrical shock sensations, seen in long COVID and vaccine-injured patients are due to the spike proteins on the COVID-19 virus’ surface. The mRNA and adenovirus vaccines similarly instruct the body to produce spike proteins.
The MIT study shows what “our clinical gut instinct” tells us is the cause of symptoms, neurologist Dr. Diane Counce told The Epoch Times.
Other factors may also be at play.
A common driver is inflammation. Inflammation occurs as immune cells clear out viruses and their proteins. Yet a constant state of inflammation is not viable for normal neural function, and neurons can become hyperreactive and damaged.
Another increasingly recognized driver is microclotting.
“The nerves form a webbing around the blood vessels … If you have clotting, then you’re not feeding the nerves correctly,” Dr. Counce said, adding that this could cause something close to “infarcts in the nerves.”
Sensory problems from microclotting often manifest alongside other symptoms, including chest pain, palpitations, and shortness of breath.
Treatments That Clear Spike Proteins
Ivermectin
Ivermectin is a first-line therapy in both treating COVID-19 infections and chronic long COVID and vaccine injuries.
N-Acetylcysteine (NAC)
N-acetylcysteine (NAC) has been shown to impair and break down spike protein. Augmented NAC may be particularly potent in its effects.
Nattokinase
Nattokinase is an enzyme derived from natto made from fermented soybeans. Japanese studies have shown that it can break down spike proteins in cell culture.
Apart from that, nattokinase also has robust anti-clotting capabilities. Therefore, the supplement can aid in the breakdown of blood clots that obstruct the sensory nerves from receiving adequate oxygen and nutrients.
Treatments That Reduce Inflammation
Intravenous Fluid Therapy
“When you have a virus, what do they first do in the hospital when you go in? Hydrate them,” Dr. Berkowitz told The Epoch Times.
He has observed that around 80 percent of his long-COVID and vaccine-injured patients would be more responsive to treatment after a few hydration sessions.
Low-Dose Naltrexone
In managing long-COVID- and vaccine-related injuries, Dr. Counce and pulmonary critical care specialist Dr. Pierre Kory have found the drug effective in treating neuropathies. Since the drug can reduce inflammation in neurons, doctors think it may have promise in treating smell-, taste-, and other related sensory problems.
Treatments That Inhibit Neural Overactivity
Dr. Berkowitz has observed that some patients’ nervous systems appear hyperreactive.
These patients are insomniac, anxious, have gastrointestinal problems, and often have neuropathic symptoms like pain and experience electric shock-like feelings. Some patients are also unresponsive to various long-COVID and vaccine-injury treatments like low-dose naltrexone.
Gabapentin
Gabapentin helps soothe the nervous system by mimicking gamma-aminobutyric acid (GABA), which works as an inhibitor in neurons.
GABA slows and blocks nervous activity, creating a calming effect. Since the gut is a major producer of GABA, patients with gut problems may benefit from gabapentin.
Stellate Ganglion Block
Stellate ganglion blocks, an invasive operation that involves an anesthetic injection into the autonomic nerves, can reset hyperactive nerves, reduce stress, and return smell and taste to affected patients.
Treatments That Repair Neurological Damage
Brain-Derived Neurotrophic Factor (BDNF)
Dr. Counce has found that patients tend to respond well to therapies that improve brain-derived neurotrophic factor (BDNF), a protein related to neural growth and survival.
Treatments That Prevent Clotting
Curcumin
Curcumin is a phytonutrient derived from the ginger plant turmeric. Studies show that curcumin has potent anti-inflammatory and anti-clotting effects. Therefore, many doctors have added curcumin to their treatment regimen, judging it to be helpful in breaking down blood clots.
Bromelain
Bromelain is an enzyme derived from pineapples. Since bromelain can digest gelatin, jelly companies advise against adding fresh pineapples to their mixtures to prevent the jelly from “setting.”
Triple Therapy
Combining anticoagulants may create a more substantial synergistic effect than using one anticoagulant alone.
Professors Resia Pretorius and Douglas Kell have found the triple combination therapy of anticoagulants—clopidogrel and aspirin, anti-platelet apixaban, and proton pump inhibitor (PPI)—to be successful in treating blood clots.